[ad_1]
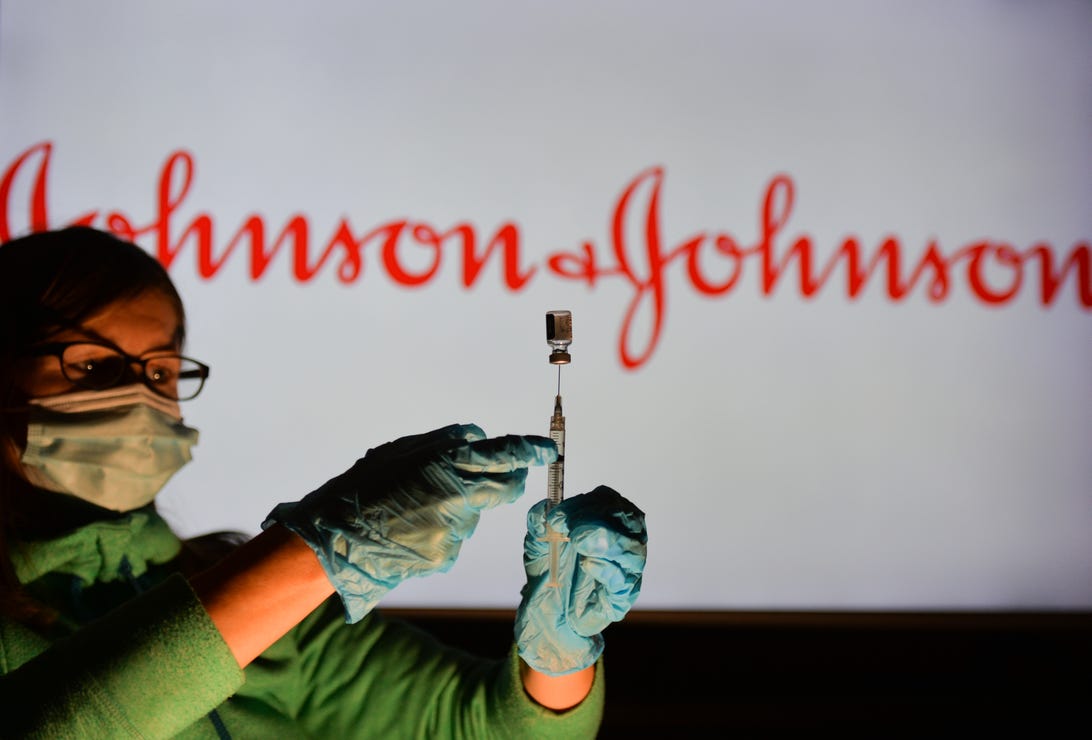
NurPhoto/Getty Images
For the latest news and information on the coronavirus pandemic, visit the WHO and CDC websites.
If you received the Johnson & Johnson COVID-19 vaccine and live in San Francisco, you can get another booster, even if you already had a second shot months ago.
Third doses for people who received Johnson & Johnson are not recommended by the US Centers for Disease Control and Prevention or authorized by the US Food and Drug Administration. Rather, it is a San Francisco Department of Health “local accommodation” to allow those who originally received the J&J to obtain a third dose.
Booster vaccines for adults and adolescents have been recommended due to the ability of the omicron variant to reduce some of the protection against infection of COVID-19 vaccines (but still maintain protection against serious illness), but they have been told people who originally opted for the one-dose vaccine to receive a second dose for months because one dose of Johnson & Johnson has a lower level of protection compared to two doses of Pfizer or Modern vaccines. (Two doses of Johnson & Johnson, however, raises vaccine protection to the same league as two doses of its mRNA cousins.)
But everyone who originally got the Johnson & Johnson vaccine should get a booster shot from Pfizer or Moderna, the CDC says, citing the rare but serious risk of blood clots after the Johnson & Johnson shot (which doesn’t happen with Pfizer or Moderna). However, if you prefer the Johnson & Johnson vaccine for any reason, it is still available. Is mix and match approach to COVID-19 vaccine boosters has been authorized by the FDA and exercised by many Americans who received boosters in recent months.
This is what you should know if you have the J&J.
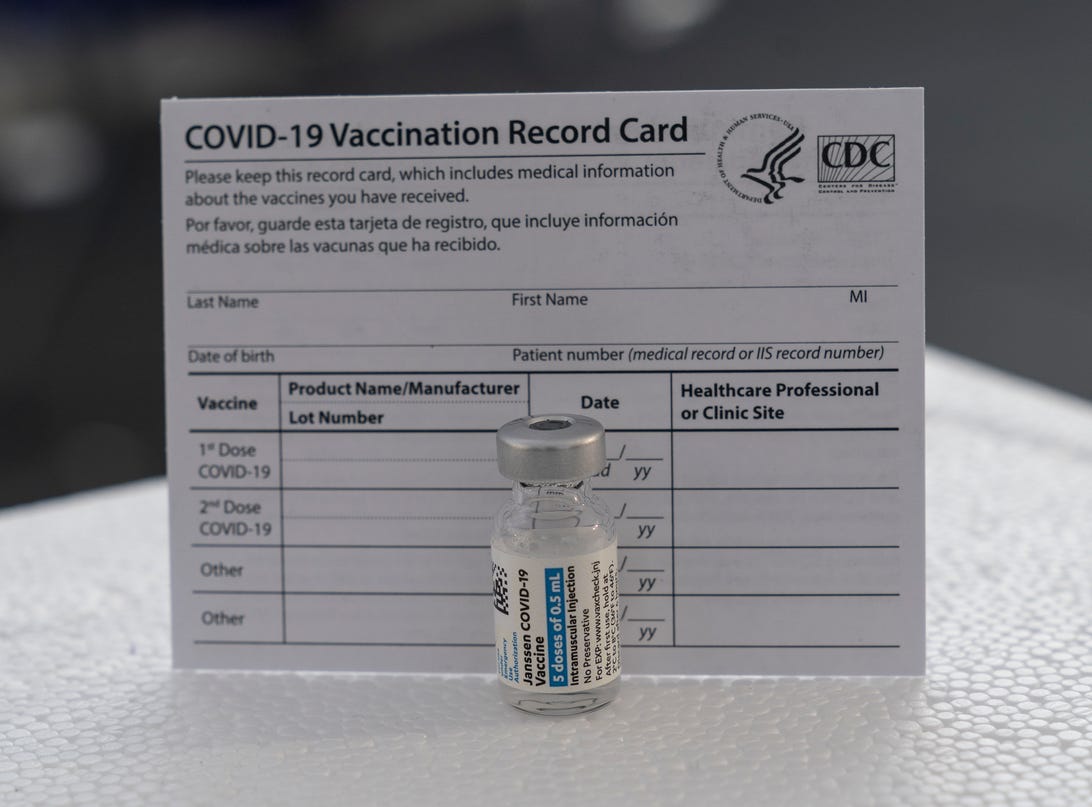
The definition of “fully vaccinated” has not changed. You are considered fully vaccinated after two doses of the Moderna or Pfizer vaccine, or one dose of Johnson & Johnson.
Pacific Press/Getty Images
Which booster should I choose if I have Johnson & Johnson?
You should get a booster from Pfizer or Moderna, the CDC says, at least two months after your Johnson & Johnson shot. Is mix and match approach for COVID-19 boosters was cleared by the FDA after early studies from the US and other countries found it to be safe and effective. In fact, some research shows that people who originally received the J&J injection have a better response to the Moderna and Pfizer booster than to another Johnson & Johnson injection.
Boosters are recommended for everyone over the age of 12 for maximum protection against omicron variantwhich appears to reduce the effectiveness of all COVID-19 vaccines, as well as protection against previous COVID-19 infections.
However, you can still receive the Johnson & Johnson booster if you wish. The reason the CDC now recommends Pfizer and Moderna over Johnson & Johnson is because none of the mRNA vaccines carry the rare but dangerous blood clotting side effect, and both also appear to be more effective than J&J. Also, vaccines are widely available in the US now, unlike earlier in the pandemic when public health advice was to get what vaccine you could as soon as you could.
Should I be concerned about blood clots if I have J&J?
If you received your Johnson & Johnson injection more than four weeks ago, you are not at increased risk of side effects, Dr. Rochelle Walensky, director of the CDC. tweeted. So if you received your Johnson & Johnson injection months ago, there is no cause for concern. Symptoms of the blood clotting disorder usually appear one to two weeks after receiving the vaccine, according to a fda fact sheet.
Although cases of the blood clotting disorder that occur after vaccination with the Johnson & Johnson and AstraZeneca vaccine are rare and have occurred in men and women (according to a CDC presentation from December, 54 cases were reported in the US through August million doses given), the risk is greatest for women ages 30 to 49, occurring in one in 100,000 women.
Vaccine-induced blood clots, TTS, also require different treatment and appear to be more fatal than other blood clots that can occur in people at higher risk because they take birth control pills, for example. TTS cases after vaccination have been fatal in 15% of cases, the FDA says, or about one in seven people. All TTS cases required hospitalization or ICU admission, nine people died, and some required post-acute care treatment after hospitalization.
If you received Johnson & Johnson in the last few weeks, know that TTS is a rare event, but symptoms include: blurred vision, severe headache, shortness of breath, change in mental status, chest pain, persistent abdominal pain , leg swelling, weakness on one side of the body, and easy bruising or small spots of blood away from the injection site, according to information from the CDC. If you experience symptoms, seek medical attention immediately.
Another side effect that people might be at increased risk of following Johnson & Johnson vaccination is Guillain-Barré syndrome, an autoimmune disorder that can also be triggered by viruses. According to a July presentation by a CDC committee, 98 cases of the syndrome were reported and one person died. In general, Guillain-Barre is more common in men and adults over the age of 50, according to the CDC.
In a December statement, Johnson & Johnson said the company “remains confident in the overall positive benefit-risk profile of its COVID-19 vaccine.”
“The safety and well-being of those who use the Johnson & Johnson vaccine remains our number one priority,” Dr. Mathai Mammen, global director of research and development, said in the statement. “We appreciate today’s discussion and look forward to working with CDC on the next steps.”
But don’t we need J&J?
Johnson & Johnson’s vaccine is easier to store than Pfizer and Moderna’s vaccines. It is also the only FDA-licensed single-dose COVID-19 vaccine, which has made it an attractive option to administer in settings such as homeless shelters, prisons, airport vaccination clinics, and for people living in remote settings. “hard to reach”. communities that may not be able to show up for a second dose. Plus, it’s an alternative to mRNA vaccines, which has contributed to some people’s hesitation about getting vaccinated (the new CDC guidance doesn’t mean you can’t get J&J now).
However, some experts on the CDC panel questioned Johnson & Johnson’s status as a single-dose treatment as a reason to recommend the vaccine, given that everyone who received it is told to get a COVID booster. -19 before those who received Moderna or Pfizer due to their lower effectiveness. If people living in communities that don’t have as much access to health care continue to get a vaccine that scientists say isn’t all that good, it could worsen health care inequalities in the country.
“It’s not just about ease,” pediatrician and CDC committee member Dr. Pablo Sanchez said in December. “It’s no longer a single dose vaccine.”
Even if the CDC’s new guidance for the Johnson & Johnson vaccine levels the playing field in the US, it may contribute to problems abroad. CDC members also raised questions Thursday about how the US advisory on Johnson & Johnson will affect distribution around the world.
“We are fortunate to have other vaccines available,” said Lynn Bahta, a CDC committee member and clinical consultant for the immunization program.
The information contained in this article is for educational and informational purposes only and is not intended as health or medical advice. Always consult a physician or other qualified health care provider regarding any questions you may have about a medical condition or health goals.

